Øyvind Time's master's thesis can help make everyday life easier for healthcare personnel who must learn how to take a fluid sample from the spinal cord or administer an epidural.

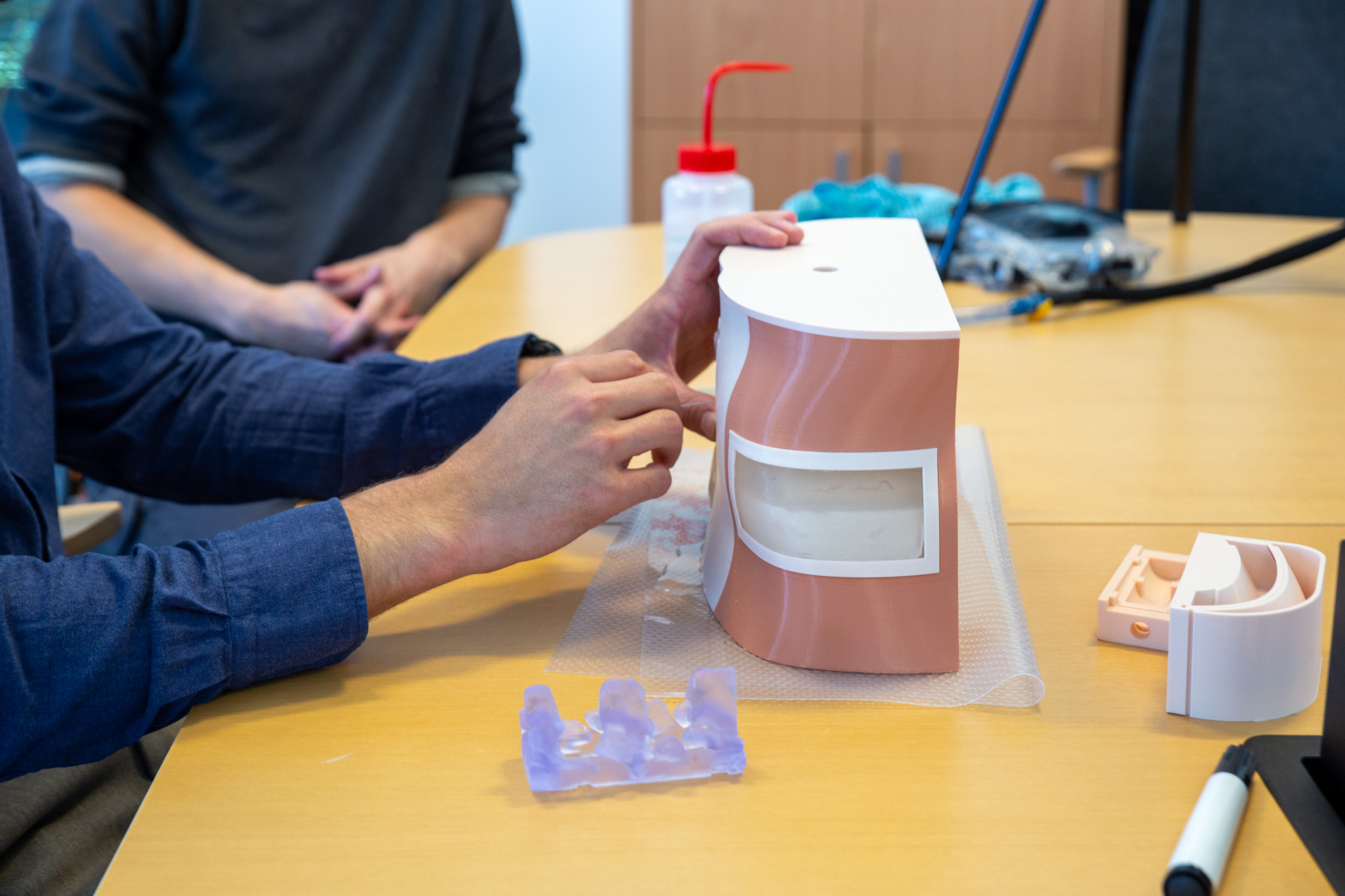
Øyvind Time fills the test model with water to mimic spinal fluid. The model is 3D printed. In the background, supervisor Eduardo Barros e Silva helps.
Doctor Thomas Bailey Tysland sticks a needle through the imitated skin layer.

Thomas Bailey Tysland feels his way to the correct cavity between the vertebrae.

The model also has fields to imitate skin on the sides of the waist. The doctor feels around to find the right point for the epidural.

Øyvind Time has spent many hours on the model. Much of the time has been spent testing the various layers that will imitate skin, muscles and fat.
To become a doctor you have to go through a long and extensive education. The medical students have practice for a total of 18 weeks. During the internship, they receive training in many medical procedures. Sometimes there is a certain risk that the patient may be injured during a medical procedure. It is therefore a goal that healthcare personnel have the opportunity to practice thoroughly before carrying out medical procedures for the first time.
Øyvind Time hopes he can contribute to that. He just handed in his master's thesis in construction and mechanical engineering. In the thesis, he has developed a practice model for healthcare personnel. The model mimics the waist area of a patient, including the lower part of the spine. The model can be used by healthcare personnel who will practice taking a fluid sample from the spinal cord (so-called spinal puncture). It can also be used for practicing putting epidurals or spinal anesthesia on patients. In both cases, a thin needle is inserted into the cavity between two vertebrae and into either the spinal canal or the epidural space. During anesthesia, the doctor finds the right point, among other things, by feeling along the side of the patient's waist, just above the hip bone.
"Skin" made of algae
The special feature of the practice model is that the various layers of the body the doctor must pass through to reach the spinal canal are very realistic. Everything from skin, muscles and fat is made from alginate, a substance that is extracted from brown algae. The "skin layer" is inserted into an anatomically realistic model, combined with skeleton. The model itself, everything from cassette to screws and skeleton, is 3D printed.
To find the right material for the layers that mimic tissue in our body, Time has had the help of supervisors from the Department of Chemistry, Bioscience and Environmental Engineering and the Department of Mechanical and Structural Engineering and Materials Science. Associate professor in biological chemistry, Eduardo Barros e Silva, has a background in biomaterials. He has helped Time find the right complexity to simulate the various tissues. Doctoral fellow Yosef Adugna has contributed in 3D design.
The result is several layers of biological material placed in a block that is inserted into the cassette. The block can easily be replaced when the material eventually dries out. The "tissue" should give healthcare personnel the same feeling as when they stick a needle through the skin of a human being.
In mid-June, only a couple of days before Øyvind Time was to hand in his master's thesis, doctor Thomas Bailey Tysland got to test the model.
"A good start!" says Tysland. He asks Time to continue working on the resistance in the layers.
"All layers that mimic tissue and skin can be made stiffer," says the doctor.
Øyvind Time has worked a lot on creating different stiffness in the layers. The layer that is supposed to imitate the epidermis (upper skin) is only two millimeters thick. Underneath, there is a layer that is supposed to imitate the dermis - the leather skin. The third layer represents the hypodermis, the subcutaneous layer. Working with recreating skin layers has been a challenge for someone who normally studies mechanical engineering.
"I have spent a lot of time trying to make this as natural as possible," he says.
The hours he has put into the master's degree project have been worth it. Through the project, he has found something he is passionate about.
"For me, this has been a perfect combination of medicine and engineering. It is something like this that I could imagine working with in the future," he says.
Much training for a cheap price
In skin-colored material, with layers of "skin" on the outside of the vertebrae, the model is very similar to a real human. Another thing that sets it apart from what is already on the market is that it is very simple and cheap to produce.
In addition, the material used for the "tissue" is very useful for practice. The material is made from brown algae found in Norwegian waters. The alginate is so flexible that it returns to its original shape after the needles have been inserted. There will be no obvious marks after the needles.
"The holes are sealed again if you use a thin needle," says associate professor Eduardo Barros e Silva.
He adds that the alginate is cheap and easy to use. Five percent of the mixture is powder from brown algae. The rest is water.
"I am very impressed by the work Øyvind has put into this project. This is the first version. There is potential here to develop an improved model that can also be used for other types of training for healthcare personnel. I look forward to following the next level of this project," he says.
Interdisciplinary work
Øyvind Time's project stands out from the rest of the master's theses of the engineering students. But Time is not the only one at the University of Stavanger (UiS) working with the use of 3D printed aids for the health sector. Doctoral fellow Yosef Adugna investigates various applications of 3D printing in medicine.
"The best thing about Øyvind's project is that it is interdisciplinary. His research builds a bridge between UiS and Stavanger University Hospital," says Adugna.
In addition to UiS and Stavanger University Hospital (SUS), the food research institute Nofima has participated in the project. The analyzes of the alginate models were done in their laboratories in Måltidets hus. The professional environment for biological chemistry is based in the same building, while SUS will soon move into new premises closeby.
"Such co-location with different actors within the same field provides benefits in interdisciplinary projects," says Camilla Normand. She is a specialist in internal medicine, and head of department for LIS doctors (doctors in specialisation) at the Reception Clinic at Stavanger University Hospital. She and colleague Svein Joar Johnsen (section chief for LIS doctors) have collaborated with UiS in this master's thesis.
"This is a super cool master's project! It is impressive to see all the details in the model," says Normand. She wants a model that works better for training than what is on the market today.
Hanne Røland Hagland, associate professor of biomedicine at UiS, has assisted in bringing together the various professional communities that have collaborated on Øyvind Time's project. She believes it is possible to develop an even better training model based on the basic work Time has done.
"Ideally, we should further develop the model in a doctoral project. It's a shame that exciting master's degree projects like this only last for three months," she concludes.
The title of Øyvind Time's master's thesis is Developing a tactile 3D-printed Lumbar spine model for clinician training in Lumbar puncture techniques.
Text og photo: Kjersti Riiber